What is Deep Vein Thrombosis?
When a clot forms in the deep vein system it is called a deep vein thrombosis, or DVT. DVTs usually occur in the lower extremities, but they can appear in other parts of the body. The venous system of the lower extremity is divided into the superficial veins, which include the great and small saphenous veins and their associated accessory tributaries and the deep venous system, which includes the femoral and popliteal veins. Intermediate veins called perforators connect them. DVT can lead to partial or complete blockage of circulation which can cause serious medical problems. Nearly 2 million Americans are affected by DVT each year.
Sometimes There Are No Warning Signs or Symptoms of DVT.
As many as 50% of patients with a DVT show no symptoms at all. These silent DVTs can resolve without treatment or may lead to complications such as a Pulmonary Embolism (PE). A PE is a dangerous condition because it can damage the lungs and other organs and is life-threatening.
Contact your doctor if you experience any of the following:
- Pain or tenderness
- Warmth
- Swelling (edema)
- Redness
Vacations are a particularly dangerous time for DVT. Travel on an airplane, car, bus or train increases your risk, especially if you have recently had surgery, are pregnant, are overweight or have a history of blood clots.
Risk of DVT should not keep you from traveling if you take these simple steps:
- Wearing compression stockings while traveling can significantly reduce your risk for DVT. These stockings help increase the circulation in your legs. Make sure to purchase medical grade stockings.
- Stay hydrated. Drink lots of water and avoid caffeine or alcohol because both are dehydrating.
- Wear loose, comfortable clothes during the trip.
- Get up out of your seat every hour or two. In an airplane, it is helpful to request an aisle seat, so it is easier to stretch out and move around. In a car, stop at a gas station or rest area and walk around every couple of hours.
- While seated, rotate your ankles, draw circles on the ground with your toes, flex your feet and toes and raise your legs slightly and hold them in the air for a few seconds.
Diagnosis of DVT
The veins of the legs are classified anatomically. The “deep” veins are within and below the muscles and the “superficial” veins are above the muscles. DVT (Deep Vein Thrombosis) is where a thrombus or clot obstructs a vein. It is a serious condition that can lead to disability and even death if the thrombus travels through the bloodstream to the lungs. When this happens, it is called a Pulmonary Embolus (PE).
Diagnosis of DVT: lower extremity ultrasound exam
Diagnosis of Pulmonary Embolus: CT Scan, Ventilation Perfusion Scan
Read What Our Patients Are Saying!
"Terrific staff and doctor, keeping the quality in the doctor /patient relationship alive and well!"
Click here to read more reviews.
Treatment of DVT
- Anticoagulation with oral or injectable medication (“blood thinners”). This is the most common treatment.
- Pharmacologic thrombolysis (infusion of drugs directly into the thrombus through a catheter that dissolve the clot)
- Surgical or minimally invasive interventions to physically remove the clot
- Compression stockings (used for small, below the knee thrombus)
- Ambulation
- IVC Filter (a small mesh filter surgically placed into the vein to prevent the clot from traveling to the lungs) if patient cannot be on blood thinners
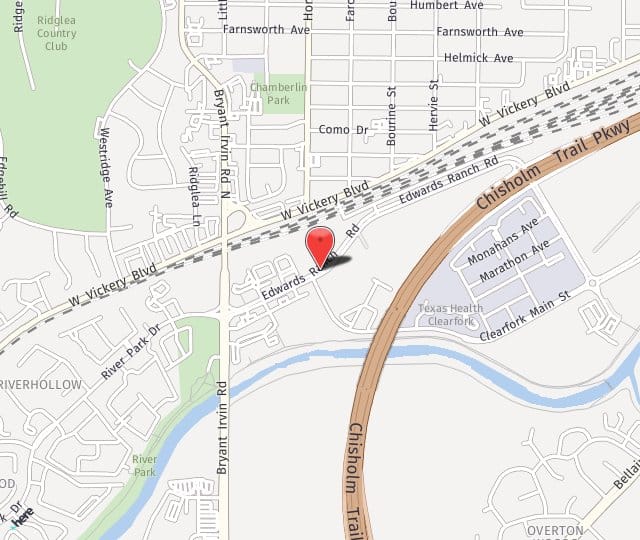
Contact Us in Fort Worth
If you are concerned about DVT, please call our Fort Worth vein doctor at 817-536-9600 or contact us online to schedule an appointment as soon as possible. Our mission is to provide you with the highest-quality medical care available in an affordable manner.